Custom Data Solutions
Explore how our comprehensive data resources can improve key business operations like network management and payment integrity programs.
Finding answers in the data
CAQH works with health plans, state agencies and other organizations to use data in new ways that improves existing processes like provider directories, provider data management systems, payment integrity programs, and third-party liability initiatives.
Let us help you:
- Do more with your own data
- Access CAQH data for deeper insights and value
- Analyze your data and provide actionable strategies
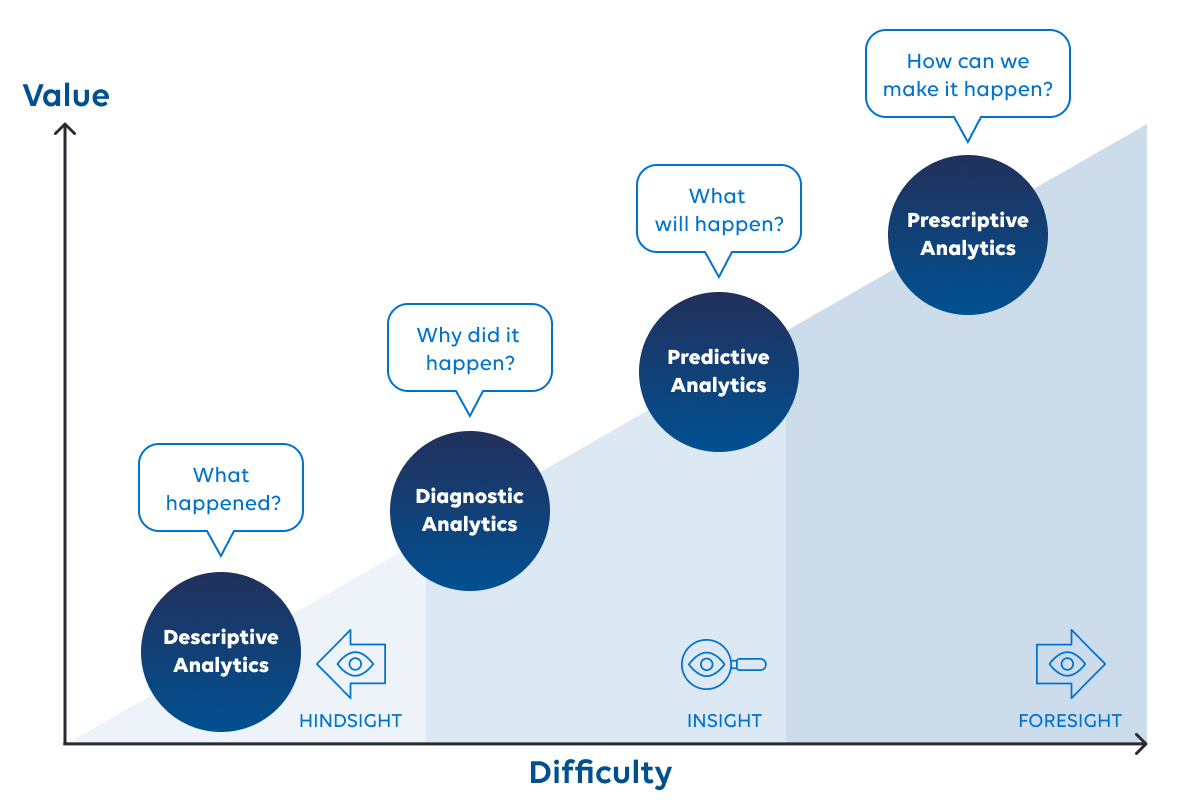
The result is improved health equity, network adequacy, referral management, member matching, data quality and more. We are focused on creating solutions that deliver the greatest insights – from descriptive analytics that show what has happened to prescriptive analytics, which show how to make something happen.
Raise overall data quality
Identify valuable supplemental data
Evaluate ongoing quality initiatives
Harnessing a Unique Resource to Deliver Powerful Results
The CAQH data platform has been designed to securely and uniquely support exceptional data quality, sophisticated analytics and targeted insights to support customer’s needs.

.png)