CORE Certification Progress Report: Measuring Market Reach
The CORE Operating Rules promote seamless, electronic sharing of large quantities of administrative data across our nation’s healthcare system quickly, cost effectively and accurately. Widespread adoption of the operating rules not only offers the promise of impressive cost savings — it also can help providers and patients worry less about “paperwork,” and focus more on care.
CORE Certification, an industry developed program, supports market adoption and tracks adherence to operating rules and their underlying standards CORE has awarded over 400 certifications to health plans, providers, and vendors across private and public markets. Achievement of CORE Certification provides organizations a means to assure, validate and demonstrate that their systems are operating in conformance with the operating rules and their underlying standards.
CORE-certified entities help to accelerate Health IT adoption by encouraging certification and full automation by their trading partners. Implementation of the operating rules and underlying standards improve industry productivity, dramatically cut administrative costs, and advance interoperability initiatives.
Below are just some of the benefits that, providers, health plans, and members receive when they engage with a CORE-certified entity.
- Providers receive a response in real-time when they verify a patient's health insurance coverage and check on the status of a claim.
- Enhances revenue cycle management during healthcare claim submission.
- Payments are processed between health plans and providers electronically and efficiently.
- Enables clear communication of next steps in the prior authorization process, including what additional documentation is needed.
- More time goes back into serving patients because the administrative burden is reduced.
In late 2016, CORE published its first annual progress report tracking the reach of CORE Certification into the nation's healthcare system. The report shares the number of lives covered by health plans that are CORE-certified, including commercial payers, Medicare Advantage and Medicaid. In 2021, CORE added measures to the repot which shares the number of providers using a CORE-certified Vendor Product in ambulatory practices and hospitals. These measures capture the reach and impact, of CORE Operating Rules on the healthcare system.
Tracking operating rule adoption is essential for accessing progress and momentum made towards nationwide commitment on topics of interoperability, streamlined data exchange, and administrative efficiencies. By measuring progress, industry can help to identify challenges that may be preventing stakeholders from adopting operating rules and underlying standards. The findings from this report prompt new strategic insights and target areas to reduce barriers.
Health Plan Marketshare
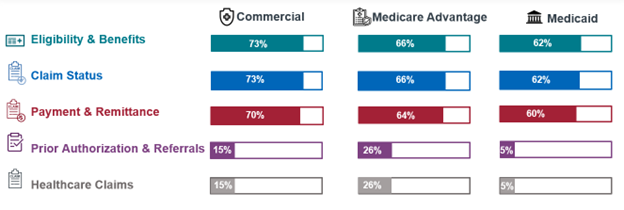
These set measures focus on the number of insured lives that are covered by CORE-certified health plans. Data from public sources, including the AIS Directory of Health Plans, Center for Medicaid and Medicare Services, and the Kaiser Family Foundation, is analyzed to determine the number of insured lives in U.S. in the commercial and public health plan markets.
In late 2016, CORE published its first progress report tracking the reach of CORE Certification into the nation’s healthcare system. The report shares the number of lives covered by health plans that are CORE-certified, including commercial payers, Medicare Advantage and Medicaid. These measures capture the reach, and thus impact, of CORE Operating Rules on the healthcare system. The next stage of the report is in development and focuses on the number of transactions conducted by providers that use CORE-certified vendors and clearinghouses.
Findings:
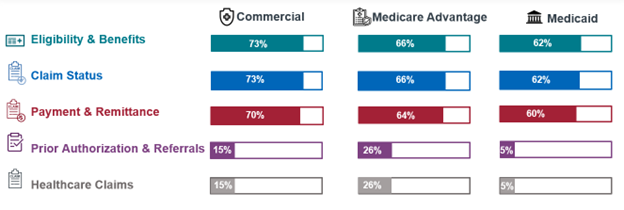
The report found that health plan CORE Certification impacts 190 million insured lives.
Insights:
- Across markets health plans and their trading partners are experiencing the efficiencies from the mandated CORE Operating Rules enabling them to save time and money.
- State agencies and health plans covering 62 percent of all Medicaid enrollees have achieved some level of CORE Certification. This compares to 73 percent for commercial health plans and 66 percent for Medicare Advantage plans.
- There is an opportunity to further promote adoption and validate implementations of electronic payments and remittances. According to findings from the CMS Compliance Review Program, the most common violation of operating rules and standards centered around the CORE Payment & Remittance Operating Rules and X12 v5010 835 transaction standard.
- Since the CORE Payment & Remittance Operating Rules were released, commercial adoption is now only 3% behind the Eligibility & Benefits and Claim Status Operating Rule sets, and only 2% behind in Medicare Advantage and Medicaid markets. This change in percentage is due to increased industry desire to transition to electronic payments and health plan adoption of all mandated operating rule sets.
- Prior Authorization adoption is increasing across health plans, with commercial and Medicare Advantage affecting 15% and 26% of covered lives. As adoption grows, vendor and clearinghouse stakeholders are certifying before health plans to meet contractual obligations. Additional industry education, guidance and policy are needed to reduce barriers and help the industry move toward more efficient prior authorization process.
Provider Marketshare
These set measures focus on the number of providers that are using a CORE-certified Electronic Health Record (EHR) or Practice Management System (PMS) in ambulatory and hospital markets. Data was taken from public and private sources, including the Office of National Coordinator Certified Health IT Developers and Editions, Definitive Healthcare, the Kaiser Family Foundation, press releases, and company profiles.
Findings:
Nearly 450,000 providers use an EHR or PMS vendor product that is CORE-certified.
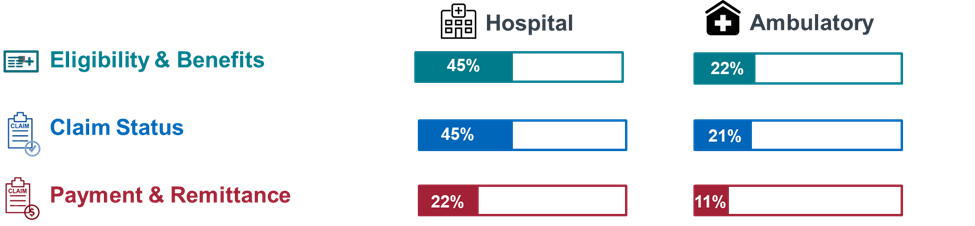
Insights:
- There is twice as much adoption of CORE-certified EHRs and PMSs in hospitals compared to ambulatory practices across all levels of certification.
- Significant work to be done to strengthen provider vendor marketshare, especially for Payment & Remittance operating rules and transactions. This includes provider education, encouraging health plans to adopt, and adjusting workflows from manual to more automated processes.
- Vendor engagement is needed to ensure providers can experience the efficiencies and cost savings afforded by the operating rules and underlying standards. Many health plans have required their vendors to be CORE-certified prior to contracting in efforts to broaden adoption, this similar approach can be leveraged by providers.
- Many health plans are requiring trading partners to pursue CORE Certification to establish direct connections, over the next few years it is expected that provider vendor adoption will grow and thus reduce costs and ensure transactional efficiencies.
Call to Action
With an ever-evolving healthcare system, the CORE mission is to drive widespread industry participation and innovation to standardize business processes for the benefit of patients, providers, and health plans. These efforts include driving greater adoption and awareness of electronic transactions and operating rules to accelerate the industry's transition to a fully digital business.
The momentum of CORE Certification highlights the commitment by insurers, providers, and vendors to effectively share electronic data in secure and meaningful ways; however, there is still more work to be done for the healthcare system to obtain the full benefits. For health plans, the operating rules mean greater efficiency and security. Provider organizations using systems that adhere to the operating rules face fewer IT and administrative hassles and can dedicate more resources to patient care. For consumers, if both plans and vendors follow them, the operating rules hold the promise of a healthcare system with fewer frustrating paperwork errors, reduced reliance on manual processes, more secure information and lower costs.
Learn how your organization can become CORE-certified or how to encourage others to pursue certification. Contact us here.
To view a list of organization that have achieved CORE Certification or pledged to become CORE-certified click here.
If you’re organization is already CORE-certified, consider participation in CORE Certification Measurement Survey. This effort will support priorities to track efficiencies and articulate the impact of operating rules have on operational and workflow improvements.
